Auckland health authorities remain cautiously optimistic that the omicron outbreak may have peaked in the country’s biggest city, even though 601 of the 856 people in hospital with covid-19 are in Auckland.
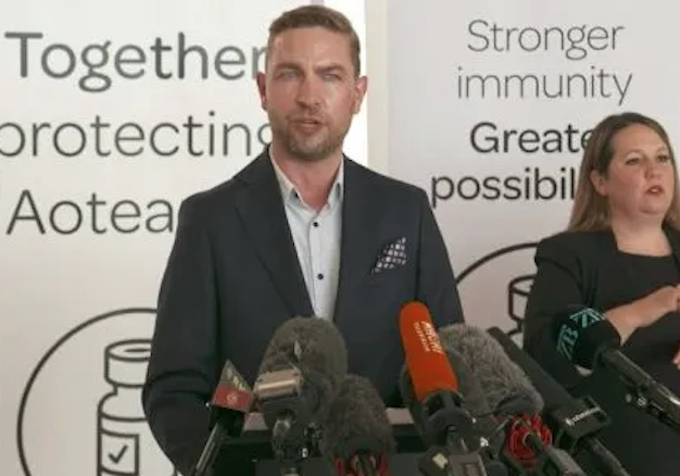
Clinical leads Dr Andrew Old, Dr Anthony Jordan and Dr Christine McIntosh at the Northern Region Health Coordination Centre gave details today on the covid-19 response.
Dr Old confirmed there were seven new deaths of people with covid-19 to report today.– the highest death toll in a day since the outbreak began.
- READ MORE: Covid-19 update: Seven new deaths reported, 20,989 new community cases
- Other NZ covid outbreak reports
Five of the deaths were in Auckland, one in Waikato, and one in the Southern region, reports the Ministry of Health.
One person was in their 50s, four were in their 70s, one was their 80s, and one person was in their 90s. Four were male and three were female.
The number of people in hospital has also risen to a record 856 people, with 20 in ICU — including 10 in Auckland — and the total new cases today is 20,989.
The total number of publicly reported covid-19 related deaths is now 98.
“It highlights that although omicron is a mild illness for many people, for some it is not,” said Dr Old.
“Every death is a tragedy and our thoughts and condolences are with the families and loved ones of the people who have passed away.”
Cautiously optimistic
He remained cautiously optimistic about the situation in Auckland.
“Our three-day rolling average of cases is about 8500 per day, which is down from a peak of about 14,000.
“Today in Auckland was the first time since this started that we had fewer people in hospital with covid at 8am this morning than we did yesterday. One day is not a trend, but certainly that is the first time.”
At Counties Manukau, the number of people coming through the door at ED is lower than it was last week. It was too early to call it, he said, but there were some encouraging signs.
Dr Old said health services in some cases were managing on a day-to-day, shift-by-shift, or hour-by-hour basis.
“I would say that we are in a crunch at the moment, so a lot of our services are operating at what’s called minimum service delivery, so a lot of those sort of more routine, corporate type activities are being put on hold.”
He said authorities knew not every case had been detected, but there was good testing coverage, with about 15 percent of people enrolled with a GP in Auckland having been tested in the past fortnight.
Relatively young
The average age of people in hospitals is still relatively young, but as the total hospitalisations have risen, more older and vulnerable members have been affected.
Dr Old said this was a trend that matched those seen overseas, and omicron tended to have a long tail, with more vulnerable and older populations more likely to be affected towards the end of outbreaks.
“People need to remain vigilant to protect those in our families and communities who are at greater risk.”
He said it was a mild illness for most people but a more severe illness for other people you could pass it on to.
Another reason to remain vigilant is the problem of long covid, he said. What was known about long covid from other variants should give pause, he said.
He urged people to keep up mask use and good hygiene as it will make a real difference as we start to come out of the outbreak and beyond.
He said authorities were expecting hospitalisations to increase again this week and they have. As a percentage of current active cases this remains about 0.5 percent, and across the whole outbreak about 1.5 percent of cases have been treated in hospital.
Dr Old said that was likely to be an overestimate, because not all infections were being reported and counted.
‘We know it’s pretty tough out there’
Dr McIntosh said that in the peak of the outbreak the whole system was feeling the strain.
“We know it’s pretty tough out there and we know that you’re doing a phenomenal job.”
She said it was not just the staff in Auckland, it was the system and workers across the whole country who were supporting the health efforts.
She said it was important that people with severe or worsening symptoms to seek help and call 111 without delay.
“Your GP and healthline are there to help you if you need it … we would rather help and help you manage a worsening illness at the earlier stages than wait until someone is really dangerously ill.”
Dr McIntosh said there were pressures within GP practices and the primary care organisation leads were met with every day, and those issues are discussed.
“But indeed it is pretty stretched … the crunch is on.”
This article is republished under a community partnership agreement with RNZ.