By Rowan Quinn, RNZ News health correspondent
Intensive care units and hospitals are getting a boost of hundreds of millions of dollars as the country moves to the covid-19 traffic light system.
Minister of Health Andrew Little announced today the government would spend $100 million upgrading buildings and facilities and $544 million for operating costs, including staffing to prepare for when covid is expected to be widespread in the community next year.
He said he had asked hospitals to identify ways of quickly increasing their intensive care beds — even though there was more than enough capacity than was likely to be needed.
- LISTEN TO RNZ MORNING REPORT: “This has always been a thing that we had to do” – Minister of Health Andrew Little (duration 7:04
- READ MORE: Other NZ covid reports
“But as the country shifts to the traffic light system, we need to make sure we can cope with the unexpected,” he said.
Four initial projects were announced.
The biggest was at West Auckland’s Waitākere Hospital, which had been given $65.1 million to build space for 30 new ward beds, six ICU beds and two negative pressure rooms.
It currently had no ICU, sending patients to North Shore Hospital instead.
Its district health board was getting a further $5 million to covert eight existing elective surgery beds to surge intensive care beds.
Bay of Plenty was given $15.5 million to create two more ICU beds and 4 high dependency unit beds. Canterbury was getting $12 million for 12 ICU beds.
‘Underdone’ before covid
Little told RNZ Morning Report: “Even well before covid, we were underdone when it comes to ICU capacity, so this has always been a thing that we had to do better on and the covid pandemic has obviously shone a light on capacity issues and and even though this most recent outbreak, we’ve actually coped remarkably well with the increasing daily case numbers, ICU capacity has been available.
“We’ve hovered between about five and I think it topped out at 11 cases at any one time in ICU.
“With the traffic light system, covid is going to move around the country. We need to know that we’ve done everything we can to maximize ICU capacity.”
Of the projects announced yesterday, three will be available in the next six months – the other is a “couple of years away”, Little said.
“These things take a little time to bring on. Early this year I had said to those responsible for putting things together, if there’s any opportunities we can take to accelerate ICU projects, let’s bring those on. This is the product of that.”
Little said Waitakere, Tauranga and Christchurch were getting more DHB capacity because they had ICU plans that could be accelerated.
Long-standing concern
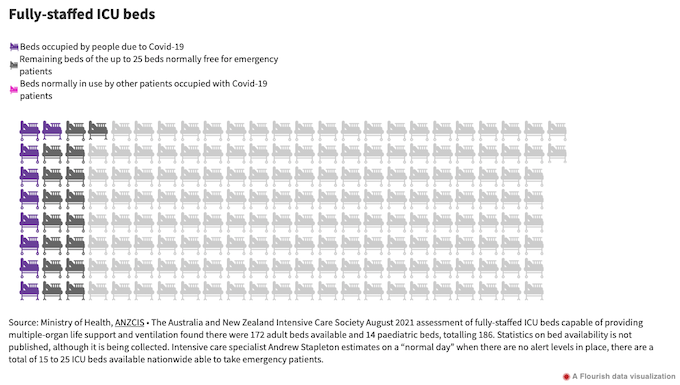
Intensive care doctors and nurses have long worried about how intensive care service around the country would cope when covid became truly endemic, saying the government was overestimating how much capacity there was.
That was because they would have to care for people with covid-19 on top of all the other usual care, for example, people who had been in car accidents, had a heart attack or who were recovering from certain serious surgeries.
They have said there is not enough capacity to cope without the high standard of care falling or some planned operations being put off.
The biggest barrier was not physical beds and equipment, but the nurses needed to staff these.
The College of Critical Care Nurses estimated the country’s hospitals were short of about 90 already and said urgent moves were needed to recruit nurses from overseas, train more here, and pay those already working better.
There were not yet details on how the new funding would help to fix the problem.
‘Delighted’ over funding
Intensive care doctor and Intensive Care Society spokesperson, Andrew Stapleton, told Morning Report the society was “delighted”.
“In the 70 years since there’s been an intensive care in New Zealand, there’s never been any targeted money in a package like this and there’s the promise of more to come, so we’re very hopeful that this is the beginning of moving in the right direction,” Stapleton said.
“It will (make a difference) in the places it’s targeted towards, so it is targeted and particularly the big win from this is Waitākere.
“So we talk about intensive care beds per 100,000. There’s roughly four for the whole of New Zealand. Waitākere’s got a population of 600,000 and no intensive care beds, and this is something we’ve been campaigning for some time.
“So, they’re going to get six intensive care beds and a 30-bed inpatient ward, and this is great news for that region.”
Intensive care beds costed about $1 million a year to run because of the staffing costs, Stapleton said.
“That gives you an idea that that is a significant boost.”
‘We’re not complaining’
While the money could have come sooner, “at this point we’re not complaining”.
Regarding covid-19, the big test was yet to come, he said.
“It’s easy to forget that Auckland, where the vast majority of covid has been, has been in level 3 lockdown until today, so what happens two weeks from now is going to be interesting to see.”
Little had earlier said 1400 nurses had completed a 4-hour online course to give them skills to help as a surge workforce if needed.
But those in the field said they would be able to provide care around the edges at best.
This article is republished under a community partnership agreement with RNZ.